April 21, 2020
By Kari Williamson at MKC Medical Management
Long before the novel coronavirus became front-page news, we knew that respiratory diseases were serious business. In fact, respiratory diseases are the leading causes of death and disability in the world. About 65 million people suffer from chronic obstructive pulmonary disease (COPD) one of the most common lung diseases and 3 million die from it each year, making it the third leading cause of death worldwide.
So, with COVID-19 adding millions of cases to these statistics worldwide, it’s safe to assume that lung-related insurance claims of all kinds will consume a bigger and bigger portion of the dollars we spend on healthcare. It makes sense, therefore, to educate ourselves about the respiratory system, about how these diseases behave, and what managing a lung-related claim might look like.
The Lungs
Let’s start with some basic, respiratory anatomy. The lungs are a pair of spongy organs on either side of the chest. The trachea takes inhaled air into the lungs through tubular branches, called bronchi. The bronchi then divide into smaller and smaller branches (bronchioles) that finally become microscopic.
The bronchioles end in clusters of microscopic air sacs called alveoli. In the alveoli, oxygen from the air is absorbed into the blood. Carbon dioxide travels from the blood as a waste product of metabolism to the alveoli, where it’s exhaled. Between the alveoli is a thin layer of cells called the interstitium, which contains blood vessels and cells that help support the alveoli.
The lungs are covered by a thin tissue layer called the pleura…the same kind of thin tissue that lines the inside of the chest cavity. A thin layer of fluid acts as a lubricant, allowing the lungs to slip smoothly as they expand and contract with each breath.
Lung Diseases
Lung disease describes anything that occurs in the lungs that inhibits them from functioning as they should. The lungs are part of a mechanism that relaxes and expands thousands of times a day to perform the oxygen and carbon dioxide exchange. Oxygen is essential for the cells throughout the body to operate properly.
There are three different subclasses of lung diseases.
- Lung tissue diseases are those that alter or have adverse effects on the structure of the lung.
- Airway diseases have adverse effects on the tubes that carry oxygen in and carbon dioxide out of the lungs.
- Lung circulation diseases negatively affect blood vessels that run throughout the lungs.
Some lung diseases may fall into more than one of these three subclasses. Additionally, there are MULTIPLE respiratory diseases. Here is an abbreviated list of some of the more common diseases. Often, a person can experience multiple diagnoses at one time.
- Chronic obstructive pulmonary disease (COPD): Damage to the lungs results in difficulty blowing air out, causing shortness of breath. Smoking is by far the most common cause of COPD.
- Emphysema: A form of COPD usually caused by smoking. The fragile walls between the lungs’ air sacs (alveoli) are damaged, trapping air in the lungs and making breathing difficult.
- Bronchitis: Can be acute or chronic. Coughing is a main symptom of acute and is typically associated with an infection. Chronic is presented as repeated, frequent episodes of productive cough, usually caused by smoking, and breathing also becomes difficult in this form of COPD.
- Pneumonia: Infection in one or both lungs. Bacteria, especially Streptococcus pneumoniae, is common, though viral pneumonia is frequently seen and would not require antibiotic therapy.
- Asthma: The lungs’ airways (bronchi) become inflamed and can spasm, causing shortness of breath and wheezing. Allergies, viral infections, or air pollution often trigger asthma symptoms.
- Pleurisy: Inflammation of the lining of the lung (pleura), which often causes pain when breathing in. Autoimmune conditions, infections, or a pulmonary embolism may cause pleurisy.
- Lung cancer: Cancer may affect almost any part of the lung. Most lung cancer is caused by smoking.
- Tuberculosis: A slowly progressive pneumonia caused by the bacteria Mycobacterium tuberculosis. Chronic cough, fever, weight loss, and night sweats are common symptoms of tuberculosis.
- Pulmonary embolism: A blood clot (usually from a vein in the leg) may break off and travel to the heart, which pumps the clot (embolus) into the lungs. Sudden shortness of breath is the most common symptom of a pulmonary embolism.
- Acute respiratory distress syndrome (ARDS): Severe, sudden injury to the lungs caused by a serious illness. Life support with mechanical ventilation is usually needed to survive until the lungs recover. This is the lung condition most closely associated with COVID-19.
About COVID-19
COVID-19 is a lung infection caused by the novel coronavirus first detected in late 2019, with symptoms ranging from mild to severe. Anyone can get COVID-19, but some individuals are more at risk for severe complications of the virus than others. There is currently no specific treatment other than supportive care available, though there are current medications being utilized in an off-label manner which are still under investigation as to their effectiveness.
The lungs are the first and main body organ affected by COVID-19. In the early days of an infection, the novel coronavirus rapidly invades cells in our lungs. COVID-19 is thought to attack the epithelial cells lining the airways which catch and clear out things like pollen and viruses flooding our airways with debris and fluids. Some studies have found that patients who experience severe disease develop pneumonia in both lungs, accompanied by symptoms like shortness of breath and the need for respiratory support. For these individuals, lung damage continues to build which can lead to respiratory failure.
Most people recover from COVID-19 within a few weeks, but it can be life-threatening. There is currently no vaccine to prevent COVID-19. The best way to prevent illness is to avoid being exposed to the virus.
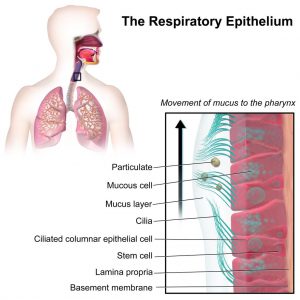
The New York Times produced this video on how the coronavirus affects the human respiratory system , including its impact on the respiratory epithelium, illustrated here.
The novel coronavirus has never before been seen in humans, so we have no immunity to it and everyone is at risk. There are some individuals who are at higher risk for severe illness if they develop COVID-19, including people aged 65 years and older, people of all ages with underlying medical conditions and others. In addition, some individuals, such as healthcare professionals and those caring for people sick with COVID-19, are more likely to get infected than others.
Respiratory and Lung Disease Claims, Including COVID-19
There’s already plenty of evidence that COVID-19 is having a huge impact on insurance and it’s safe to assume that the virus will possibly affect virtually every line of coverage for years to come in addition to affecting the cost of health insurance. If individuals elect to forgo insurance coverage due to cost, then they are possibly less likely to receive appropriate medical care for underlying health conditions which will make them at higher risk for contracting the virus.
First, some claim basics.
- Inhaling irritants such as dust and fumes can cause respiratory and lung conditions and can also worsen pre-existing conditions. For example, exposure to asbestos dust can cause asbestosis, lung cancer or other asbestos-related diseases to develop, and exposure to silica can cause silicosis. Breathing in coal dust, spores, dust from textiles, fumes from welding, smelting, pottery-making and plastics manufacturing, spores from grain and wool, and mould from hay can also cause respiratory diseases.
- Vapors from chemicals and gases such as formaldehyde, chlorine and ammonia are particularly dangerous. Other harmful fumes can be found in paints, acids and solvents, cleaning materials, lacquers and pesticides.
- Some employees with a pre-existing condition may also find their symptoms worsen because of an employer’s poor health and safety.
- Industrial disease claims are often more complicated than other personal injury claims. The cause of the illness or injury could have occurred years earlier and expert evidence may be needed to prove a link between the illness and employment.
Here’s a look at some of the issues that will play out over the next several months.
Comprehensive General Liability Insurance (CGL) policies generally cover bodily injury and property damage caused to third parties on insured premises. Allegations that an insured caused a guest, customer or third party harm by failing to exercise reasonable care in implementing, enforcing or warning of the risk of potential exposure to the coronavirus could be covered by a CGL policy. To the extent that a guest, customer or third party alleged bodily injury as a result of an insured’s negligence, we would expect to see coverage absent a specific exclusion.
Under Workers Compensation Insurance (WC), bodily injury claims brought by an insured’s employees (as opposed to third parties) may be covered by a WC policy. However, most WC policies do not cover “ordinary diseases of life” (diseases to which the general public are also exposed). There is an exception if an employee can establish a direct causal connection to the workplace but it is not clear whether that exception would apply absent a unique relationship with the virus (e.g., there may be a direct relationship for first responders, laboratory workers, etc. that are required to work with the virus as part of their jobs). If the employer does not provide the appropriate PPE (protective protective equipment) then they may be held liable. Under OSHA employers have the obligation to protect their employees.
For workers who have a pre-existing lung condition, such as asthma, they may be entitled to workers’ compensation benefits if their current job triggered or exacerbated their disease. For example, if their lung condition had been manageable but worsened at their current workplace, even if it was present before exposure at work, they may still have a valid claim for compensation. Again, it is important to understand that symptoms from asthma may be “latent,” which means that they may not surface immediately. Employees who have a pre-existing medical condition that is worsened by current workplace conditions will find it critical to have medical opinions that demonstrate their current, aggravated condition.
COVID-19 Claim Take-Aways
While the final effects of Covid-19 remain to be seen, the virus has shown us that it can be deadly. It will have devastating effects on the economy, as well as the insurance industry. Even individuals who never contract the virus will feel the impact in one way or another — and life as we have known it will change.
One last reminder. In examining any claim, it’s important to assess any effect that underlying conditions have on the progress of the virus on a patient. Analysis of pre-existing conditions is a complex issue that comes into play in every illness or injury claim — whether heart disease and diabetes or a motor vehicle accident.
About the Author
Kari Williamson, BS, RN, LNCC, CCM, is a nationally recognized Legal Nurse Consultant and the owner and chief executive of MKC Medical Management. She founded MKC in 1995 to help business owners and managers, lawyers, insurance adjusters, and others better understand the facts of complex medical claims and disputes. Contact Kari at 865-850-9349 or kari@mkcmedicalmanagement.com.